Breast cancer screening
Screening through mammography has demonstrated a reduction in breast cancer mortality by 20-40%. Nevertheless, existing breast cancer screening programmes are primarily predicated on age, generally excluding women under the age of 50 or 45 from regular screenings. The efficacy and potential drawbacks of screening women under 50 are subjects of ongoing debate, resulting in a lack of comprehensive screening recommendations for this demographic. The implementation of personalised risk assessments is essential to pinpoint women who benefit from earlier screening initiation.
Moreover, for women above 50 at heightened risk, the conventional screening frequency of 2–3 years might not be ideal, often overlooking cases that could have been identified earlier.
Colorectal cancer screening
Incorporating polygenic risk score testing into the colorectal cancer screening strategy offers a refined approach to assessing risk. This genetic insight, combined with age and gender data, provides a comprehensive risk profile that informs personalised screening protocols. This enables more precise recommendations regarding the age at which to initiate colorectal cancer screening and the preferred methods. Tailoring screening recommendations to an individual’s unique genetic composition signifies a key advancement in the global endeavour towards precision medicine in cancer prevention.
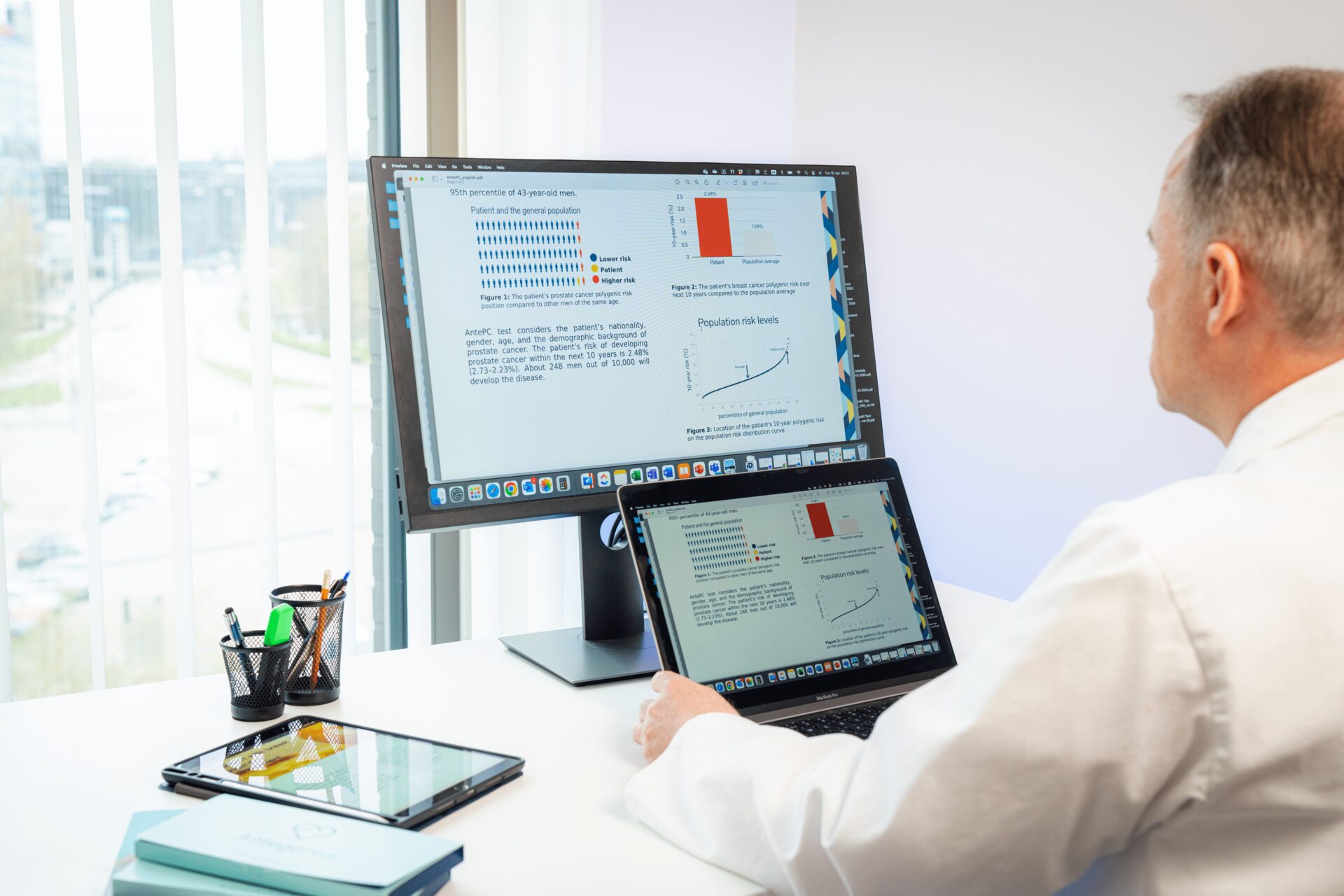
Prostate cancer screening
The European Association of Urology (EAU) guidelines for prostate cancer emphasise individual early detection and risk assessment, particularly for men with specific risk factors such as age, family history of prostate cancer, men of African descent, and carriers of BRCA2 mutations. The guidelines advocate for a personalised approach to early detection and screening, including the use of PSA testing and digital rectal examination (DRE), while also considering the patient’s life expectancy and co-morbidities. The prostate cancer PRS test is an additional important factor characterising prostate cancer risk that must be considered in individual risk assessments and subsequent screening decisions.